By Sunil Bochare MD
Pediatric Urgent Care Physician, University Hospital, San Antonio, Texas
sunil.bochare@uhtx.com
AI is rapidly becoming a tangible reality in healthcare, offering clinicians promising tools for enhancing diagnostic accuracy, streamlining workflows, and improving patient outcomes. This potential is crucial for common, challenging conditions like urinary tract infections (UTI), which alone account for approximately eight million office/emergency visits and one million hospitalizations annually in the US. However, inaccuracies and delays in UTI diagnosis lead to increased morbidity and mortality. Diagnostic errors significantly contribute to critical issues such as antimicrobial resistance (AMR)—affecting over 2.8 million people and linked to ~35,000 deaths annually in the US per the CDC, exacerbated by pathogens like extended-spectrum beta-lactamase (ESBL)-producing organisms—and increase risks for major complications and clinically significant secondary infections like clostridium difficile.
Addressing this complex challenge with its significant clinical and public health ramifications, this article explores the current state of AI tools designed to support clinicians in UTI management, reviews the evolution of these AI applications, and discusses ongoing work in this critical area.
The Evolving Story of AI in UTI Diagnostics: A Look Back
The journey of applying AI to improve UTI diagnosis reveals a progression from exploring predictive potential to tackling practical implementation challenges:
- Early Exploration: Predicting UTIs in the Complex ED Setting (Taylor et al., 2018)1
Recognizing the high rate of diagnostic errors for UTIs in busy Emergency Departments (EDs), early research leveraged EHR data. Taylor et al. tested multiple machine learning algorithms (like XGBoost) on a large dataset, using hundreds of variables. They found AI could predict positive urine cultures with high accuracy (AUC up to 0.904 for the best model) and showed significantly better specificity than clinician judgment proxies, suggesting AI could reduce false-positive diagnoses. This established the potential for AI in complex UTI prediction. - Focusing on Efficiency: Reducing Lab Workload (Burton et al., 2019)2
The focus then shifted to the practical problem of excessive negative urine cultures overwhelming labs. Burton et al. used a massive dataset (>200,000 reports) to compare simple lab rules (WBC/Bacteria thresholds) against machine learning models. A key finding was that patient populations matter; pregnant patients and young children required separate analysis. Their best AI solution used three separate XGBoost models for different groups, offering high sensitivity (~95%) and a potential 41% workload reduction, significantly outperforming simple rules. This highlighted the need for data stratification and revealed the practical challenges of implementing complex AI versus simpler, interpretable rules. - Taking Stock: Synthesizing the Evidence (Goździkiewicz et al., 2022)3
A literature review by Goździkiewicz et al. confirmed that various AI models showed high performance in retrospective studies, with urinalysis components being key predictors. However, it noted no single “best” algorithm had emerged and stressed the need for prospective studies to validate these findings before widespread clinical use, highlighting the gap between research potential and validated tools. - Maturing Towards Implementation: Standardization and Interpretability (Seheult et al., 2023)4
More recently, work has focused on real-world, multi-site implementation. Seheult et al. developed the “PittUDT” algorithm using a decision tree – chosen for its human-interpretability and ease of LIS implementation. They emphasized rigorous data cleansing and standardization across five hospital labs. Their simpler, rule-based AI achieved high negative predictive value (>90%) and could reduce cultures by 30-60% with a low false-negative rate (<5%), demonstrating a practical approach for multi-site deployment and ongoing quality monitoring.
Current AI Tools Augmenting the Clinician’s Toolkit
Beyond UTI-specific research, several AI tools are emerging to assist clinicians more broadly:
- Ambient Clinical Intelligence: AI systems that listen to patient encounters (with consent) to auto-generate clinical notes, reducing documentation burden.
- Intelligent Medical Imaging: AI algorithms assisting in analyzing X-rays, CTs, etc., to potentially speed up detection of findings.
- Clinical Decision Support (CDS): AI-driven CDS analyzing patient data to provide evidence-based recommendations, flag risks (like sepsis), and suggest differential diagnoses, moving beyond simpler rule-based alerts.
Translating Research into Practice: Developing and Validating Clinical Workflows
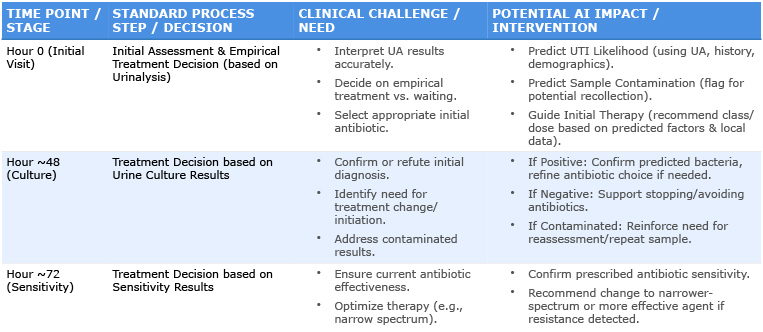
The drive to translate research into practice is leading to the next frontier: integrating AI capabilities seamlessly into clinical workflows and rigorously validating their real-world performance. Building upon the foundational research, efforts are underway to create and test practical, point-of-care tools.
One such effort is UTIwizard, a startup initiative involving a collaborative team (including the author) of clinicians, informaticists, and data scientists. Our focus is developing a machine learning system for more holistic UTI management in adults and children before culture results are available. Using urinalysis, clinical history, and demographics from extensive datasets—representing over 100,000 patient encounters analyzed over the course of four years so far—our models aim to predict contamination risk, UTI likelihood, probable bacterial species, and antimicrobial resistance patterns to guide antibiotic selection. This extensive data foundation emphasizes the robustness of our analysis compared to previously mentioned studies. Our work aligns with and helps validate prior research findings, demonstrating robustness across different datasets. The goal is to translate this multi-faceted AI approach into a practical clinical decision support tool to improve diagnostic accuracy, speed appropriate treatment, and combat AMR.
The Road Ahead: Promise and Prudence
The future holds exciting possibilities for AI in clinical practice. However, responsible adoption requires careful consideration:
- Validation and Trust: AI tools need rigorous validation, including prospective studies, using diverse datasets relevant to the intended patient populations (both adult and pediatric) to ensure accuracy, safety, and equity.
- Integration: Seamless integration into existing EHRs and clinical workflows is crucial for usability and adoption.
- Ethics and Privacy: Robust safeguards for patient data privacy and ethical guidelines for AI deployment are paramount.
- The Human Element: AI should be viewed as an assistant – a tool to augment, not replace, the clinician’s judgment, experience, and the vital patient relationship. Active clinician involvement in the development, validation, and implementation process is essential for creating truly useful and trusted solutions.
Bridging the Gap: The Clinician’s Role in the AI Revolution
For many clinicians, the drive to improve patient care stems from daily practice – seeing the patterns and understanding the nuances behind the data we generate. While complex analysis tools were once out of reach for many without coding expertise, a new generation of more intuitive platforms (including AI assistants, Python, RStudio) is democratizing data science. This shift empowers clinicians, with their invaluable domain knowledge, to directly explore data and collaborate more effectively with data scientists. This vital partnership – combining clinical context with technical skill – helps avoid flawed assumptions and ensures AI tools are built to be clinically relevant, practical, and grounded in the realities of patient care. This journey towards leveraging AI to bridge clinical insights with data-driven discovery is one many, including myself, are now undertaking.
Conclusion
AI is poised to become an increasingly valuable partner for clinicians. By automating tasks, providing data-driven insights, and supporting complex decision-making for common conditions like UTIs, these technologies offer the potential to enhance efficiency, improve diagnostic precision, and support high-quality, timely patient care for patients of all ages. Critically, the increasing accessibility of data tools empowers clinicians to play a central role in guiding AI development, ensuring that innovations are grounded in clinical reality. For colleagues interested in exploring how these newer data analysis tools can be applied to clinical questions, our team at UTIwizard welcomes connection and opportunities for shared learning. As clinicians, staying informed and engaged with these developments, including innovative efforts to rigorously validate and translate these tools into practice by collaborative groups, will be key to navigating and shaping the future of patient care.
References
- Taylor RA, Moore CL, Cheung K-H, Brandt C. Predicting urinary tract infections in the emergency department with machine learning. PLoS ONE. 2018 Mar 7;13(3):e0194085. doi: 10.1371/journal.pone.0194085.
- Burton RJ, Albur M, Eberl M, Cuff SM. Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak. 2019 Aug 23;19(1):171. doi: 10.1186/s12911-019-0878-9.
- Goździkiewicz N, Zwolińska D, Polak-Jonkisz D. The Use of Artificial Intelligence Algorithms in the Diagnosis of Urinary Tract Infections-A Literature Review. J Clin Med. 2022 May 12;11(10):2734. doi: 10.3390/jcm11102734.
- Seheult JN, Stram MN, Ondras M, Contis L, Pontzer RE, Hardy S, Wertz W, Baxter CM, Kip PL, Snyder GM, Pasculle AW. Development, Evaluation, and Multisite Deployment of a Machine Learning Decision Tree Algorithm To Optimize Urinalysis Parameters for Predicting Urine Culture Positivity. J Clin Microbiol. 2023 May 25;61(6):e0029123. doi: 10.1128/jcm.00291-23. Epub 2023 May 25.
Disclosures
Dr. Sunil Bochare is a Pediatric Urgent Care Physician at University Hospital, San Antonio, Texas. He is also the CEO and Founder of UTIwizard Inc., the startup initiative mentioned in this article. UTIwizard Inc. is an independent entity and is not affiliated with University Health. Dr. Bochare has a financial interest in UTIwizard Inc.



